Evidence that Improves the Human Condition
My research integrates biological, behavioral, and social perspectives to understand and address complex health challenges across the lifespan. I lead interdisciplinary teams and multi-site collaborations focused on substance use, nutrition, and adversity in rural and underserved populations.
Substance Use & Substance Use Disorders
Substance use and substance use disorders affect millions of Americans and have profound social and biological consequences across the life course. In the United States alone, an estimated 46 million adults had a substance use disorder in the previous year, and nearly one in four children lives with a parent who has a substance use disorder. Alcohol use disorder is the most prevalent use disorder, which affects as much as 10% of the US population.
Overdose deaths are often concentrated among working‑age adults. These deaths remain a major public health crisis. The crisis was initially driven by pharmaceutical marketing campaigns and subsequent prescribing of opioid pain medications. Many states have taken action to monitor and reduce prescribing practices and to seek legal action against opioid pain pharmaceutical manufacturers. Indeed, I was part of this legal action in the state of Oklahoma, aiding in the plan to abate the crisis. In recent years, the crisis has been driven by fentanyl use, a far more dangerous opioid. More than 100,000 drug overdoses occurred annually through 2023; however, initial projections indicate year-on-year decreases on overdose deaths in 2024 and 2025.
The loss of life from the opioid crisis reverberates through families and communities: from 2011 to 2021, more than 320,000 U.S. children lost a parent to a drug overdose. Over the decade of observation, the rate of parental loss more than doubled. Moreover, the rate of loss was more likely to impact American Indian children. These losses underscore how substance use and overdose epidemics intersect with childhood adversity and long‑term health trajectories.
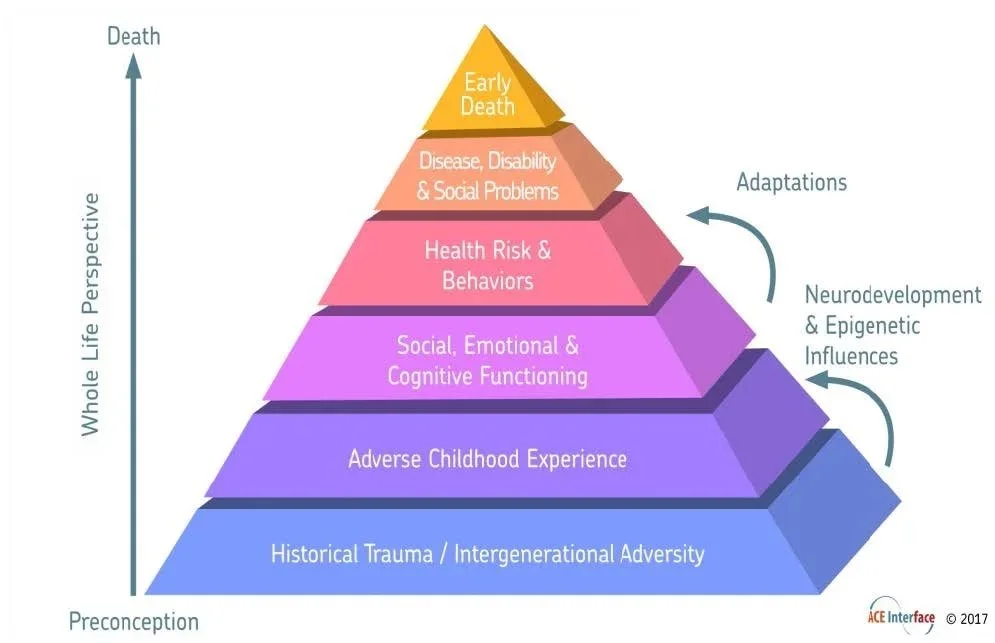
This multigenerational burden of substance use and overdose is just one example of how substance use shapes the conditions of early life exposure and adversity that profoundly influence developmental pathways and health outcomes.
Adversity
Early-life adversity includes parental substance use, household instability, neglect, and abuse. These experiences profoundly shape children’s developmental trajectories and long-term health outcomes. In the U.S., adversity affects more than 1 in 5 children before age 18.
However, adversity does not end at 18. Many individuals continue to experience family dysfunction, economic stress, and interpersonal trauma into adulthood, which can exacerbate substance use risk and interfere with recovery. Our ongoing projects measure adult exposure to adversity and household dysfunction during periods of substance use and recovery, capturing how persistent environmental stress interacts with biological and behavioral mechanisms to influence health outcomes across the lifespan.
Biologically, exposure to adversity disrupts stress-response regulation, immune function, and subsequently impacts brain development. These exposures also shaping social and behavioral pathways, creating lasting effects on mental and physical health. Shout out to my colleagues in the PACEs lab, who are working to identify social and behavioral mechanisms that interrupt the impact of trauma.
These impact of adversity often interact with environmental and community factors, meaning that individuals in rural or underserved populations may experience compounded risk. Understanding how early-life and ongoing adversity influence health highlights the need for research that integrates social, behavioral, and biological perspectives to address disparate outcomes between rural and urban communities.
Rural & Underserved Communities
People living in rural areas of the United States experience higher rates of morbidity and mortality across a range of health conditions compared with their urban counterparts, reflecting deep structural and systemic disparities. About 1 in 5 Americans resides in a rural community. Rural residents are at greater risk of premature death than people living in urban areas from the five leading causes of death: heart disease, cancer, stroke, chronic lower respiratory disease, and unintentional injury. Rural residents have higher rates of risk factors which underlie these higher morbidity and mortality numbers: higher rates of smoking, obesity, and limited access to preventive care that contribute to these disparities.
Access to health services is a persistent barrier in rural areas. Geographic isolation, fewer healthcare providers, hospital and clinic closures, and lower insurance coverage contribute to poorer care access and worse outcomes relative to urban populations. These gaps are particularly pronounced for behavioral health and chronic disease management, amplifying the long‑term effects of early-life adversity and substance use on health trajectories.
Our work engages these disparities directly by integrating biological, behavioral, and social perspectives to understand the mechanisms driving rural health inequities and to inform interventions tailored to rural and underserved contexts. Most of our projects operate under the operational umbrella and in collaboration with OSU Center for Rural Health, who support workforce development, community health needs assessment, and telehealth and healthcare delivery innovations designed to improve access and equity in rural Oklahoma and beyond.
Life Changing Research
Learn more about our projects that are applied to address these topics. Our portfolio includes the HEALthy Brain and Child Development Study, the Center for Integrative Research on Childhood Adversity, Community Coalition Teams, and Evaluation and Technical Assistance Teams.